Pelvic organ prolapse can be an uncomfortable topic to talk about, which is completely understandable. While pelvic organ prolapse isn’t life-threatening, it can cause a great deal of pain and discomfort for those who struggle with it. When the pelvic floor can no longer support the pelvic organs - like the vagina, cervix, uterus, bladder, urethra, and rectum - your medical provider may diagnose you with pelvic organ prolapse (POP).
If you haven’t been diagnosed, you might find the list of pelvic organ prolapse symptoms below helpful to see if you should get checked out. We’ve also outlined the different treatment options for pelvic organ prolapse, ranging from lifestyle changes to surgery. If you’ve heard that surgery is the only option, then you’ll be happy to find out that there are actually several other less-invasive options available. But first, let’s look at pelvic organ prolapse symptoms.
What are some common pelvic organ prolapse symptoms?
It’s important to consider that while there are many pelvic organ prolapse symptoms, the symptoms and their severity are going to vary from person to person. Below are the most common symptoms of POP as reported by those struggling with the condition.
- Seeing or feeling a bulge coming out of the vagina
- Pressure, discomfort, fullness, or achiness in the pelvic region
- Heaviness in lower stomach and genitals
- Pelvic pressure that increases when standing, coughing, or later in the day
- Incontinence (leaking urine)
- Problems peeing or during bowel movements (bladder not emptying enough, etc.)
- Problems when inserting tampons or menstrual cups
- Discomfort or numbness during sex
In some mild cases, there are no symptoms and pelvic organ prolapse is found during an internal examination for another reason. In that case, some people can go on living with it without knowing that it’s a problem because they don’t feel any pain or discomfort.
Does pelvic organ prolapse go away?
Unfortunately, it’s not likely that pelvic organ prolapse will go away. However, according to Informed Health, “Most women only have a mild prolapse that may even go away again after a few months or years.” Although this may be the case for some women, in many cases it actually gets worse over time without treatment.
Do you have to get surgery for pelvic organ prolapse?
One of the most common misconceptions about pelvic organ prolapse is that surgery is the only option for treatment. This is often a scary thought for women who have just been diagnosed with POP, but it’s certainly not true. While surgery is an option for some women, especially for those in more severe stages of pelvic organ prolapse, there are several other options available that you can discuss with your provider.
Treatment options for pelvic organ prolapse
Lifestyle changes
In some cases, the prolapse is mild and minimally bothersome so some women might find that they can simply make some lifestyle changes to relieve most of their discomfort. Some of these changes include losing weight, preventing constipation, and avoiding heavy lifting. These will all put less stress on the prolapse and should be considered as viable options for reducing the amount of discomfort present. For those who have a more severe prolapse, these options may not relieve all of the pelvic organ prolapse symptoms, but the changes can be made in conjunction with other treatments which will be outlined below.
Pelvic floor exercises
There are specific exercises that can be done to not just prevent, but also to manage pelvic organ prolapse. These are best done, or at least initiated, with a professional physiotherapist to ensure that you’re doing them correctly and not causing further harm to your pelvic floor.
Pelvic floor exercises, also commonly known as Kegel exercises, strengthen the pelvic floor muscles which help to support your pelvic organs from descending. While these can be helpful for prevention, they can also help slow the progression of pelvic organ prolapse for those with mild severity. The downside of pelvic floor exercises is that they require a lot of commitment and consistency. Therefore, it may take some time for results to show.
Vaginal pessaries
A vaginal pessary is a removable device that is inserted into the vagina to support the pelvic organs. Many times this is the first treatment your doctor will discuss with you, as it’s not as invasive as surgery but can be very successful in easing discomfort. You may be surprised to find that there are many different sizes and styles of pessaries, so you and your doctor will need to find one that fits your needs best. With that being said however, there are many women who cannot be fitted for vaginal pessaries. Their body will reject the pessary because it is a foreign object that is put inside the body, or the prolapse is too severe for a pessary and it will fall out of place. Once inserted, a pessary can generally stay in the vagina for up to three months, but regular removal and cleaning is recommended to avoid infection.
A pessary may be an option for you, but many women find that pessaries comes with a lot of side effects, including include pain, discomfort, bleeding, bad odor, and infections. Therefore, these women tend to look for other treatment options that are less invasive.
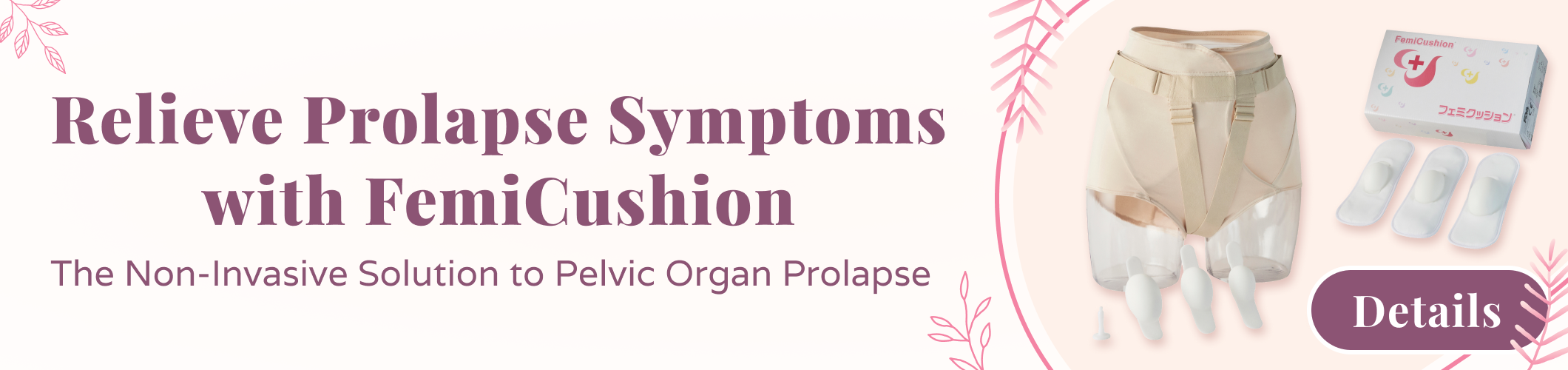
FemiCusion
One of the most unique products is FemiCushion, a medical-grade prolapse support garment that can be worn straight out of the box. It is non-invasive, which means that there are few risks or side effects when using FemiCushion. It’s designed to look just like knickers, making it discreet. At the same time, it offers the benefits of a pessary with its patented external pessary system designed to provide immediate relief. Additionally, FemiCusion has been proven to reduce the following symptoms to help improve quality of life with continuous use:
- Pain or discomfort in lower abdomen
- Feeling a lump or bulge in pelvic area
- Visual lump or bulge outside the vagina
If you’re interested in exploring this option some more, you can find more information and see the available FemiCushion options here.
Surgery
If none of the less invasive options outlined above are working, then surgery is often recommended. Reconstructive surgery is most commonly used and is typically done through the vagina or the abdomen. During surgery, your own body tissue or a synthetic mesh will be used to repair the prolapse and build pelvic floor support. For women who no longer have vaginal intercourse, an obliterative surgery can be done. In this case, all or part of the vagina is closed to keep the organs from descending.
As you can see, there are many different options to relieve pelvic organ prolapse symptoms. Most of them are non-invasive and can greatly improve your comfort and pain levels, giving you a better quality of life.
Disclaimer: The information on this site is not intended or implied to be a substitute for professional medical advice or diagnosis. All content, including text, graphics, images, and information, contained on or available through this website is for informational purposes only.