Pelvic Organ Prolapse (POP) can have a huge impact on your quality of life. If you have this condition, you’re not alone - about 1 in 4 women struggle with POP.[1] Fortunately, there are treatments available to help you manage the unwanted side effects. The first step to reclaiming your life from POP is to make an appointment with a doctor. You may be worried about discussing it with anyone (even a medical professional), so let us ease your mind and walk you through your first doctor’s visit.
In this article we will go over:
- What Doctor to See for Pelvic Organ Prolapse
- What to Expect at Your First Visit
- What to Ask Your Doctor
Note: The information below shouldn't be used to replace the advice of a qualified and licensed doctor or other health care provider and should be used for informational purposes only.
What Doctor to See for Pelvic Organ Prolapse
Deciding what doctor to see for a POP consultation can be tricky. In general, any women’s health care doctor or provider is likely a good place to start, but receiving a proper diagnosis depends on his or her experience with treating POP. Common doctors and providers that take POP patients include:
- Urogynecologists
- Gynecologists
- Obstetrician-Gynecologists (OB-GYNs)
- Nurse Practitioners (NPs)
- Physician’s Assistants (PAs)
- Licensed Midwives (LMs)
All of the providers listed above are likely able to make a diagnosis, counsel you on your options, and offer some form of treatment.
Urogynecologists are the most specialized in this field but it may be difficult to get an appointment without a referral from another provider. Licensed midwives, nurse practitioners, and physician's assistants should be able to accomplish everything you need during your first visit, including reviewing and prescribing natural methods. If you decide to have prolapse surgery, your provider will refer you to an appropriate surgeon.
Whichever provider you meet with, the first visit is the best time to talk about your condition and explore different treatment options. Keep in mind every provider’s training and experience is different, so just be open and honest about your questions and concerns so that the best treatment can be prescribed for your POP condition.
What to Expect at Your First Visit
The first visit is an important time to let your doctor know what you are dealing with and ask questions. You may also discuss a diagnosis and treatment options. Additionally, you may be scheduled for follow-up appointments and tests depending on the diagnosis.
When being diagnosed, your doctor will check to see what type of prolapse you have. There are several types of POP and two or more may happen at the same time. Knowing which pelvic organs are dropping will help the doctor suggest the best treatment option.
Not only will the doctor diagnose the type of POP, but how severe it is. There are different ways severity can be measured. One common way is to check how far outside of the vagina the prolapsing organ bulges.[2]
The doctor's diagnosis is made by considering your symptoms, performing a pelvic exam, and possibly doing additional testing. The pelvic exam typically lasts a few minutes and may be conducted while laying down or standing.
During a pelvic exam, the doctor may look inside the vagina with a speculum to see what organs are prolapsing and how severe the condition is. The doctor may also use one or two fingers to feel the inside of the vagina to check the strength of the pelvic floor muscles.
If the doctor thinks it is necessary, you may be scheduled for additional testing. Common pelvic organ prolapse tests include CT scan, cystoscopy, defecography, intravenous pyelogram (IVP) procedure, pelvic floor MRI, pelvic ultrasound, and urodynamics.
What to Ask Your Doctor about Pelvic Organ Prolapse
Be prepared to answer many questions about your pelvic symptoms and personal life. These questions may be sensitive and can be difficult to talk about. Sometimes it’s hard to find the right words to explain your symptoms. Just remember that your provider wants to help you.
If it is difficult to put your symptoms into words, here are some common ways to describe them:
- Pressure or bulging inside the vagina
- Feeling like something is falling out
- Feeling like something is pushing against you when sitting
- Discomfort in the abdomen
- Frequent urine “leaking” especially when laughing, coughing, sneezing, jumping, etc.
- Frequent urge to urinate
- Constipation or inability to completely empty the bowels
- Bleeding and spotting
- Symptoms becoming stronger in the afternoon or evening
- Decreased sex drive or ability to have sex (less common symptom)
As personal as these symptoms may be for you, talking about them will help your doctor understand what treatment is best for you.
Throughout the appointment, your doctor will be able to answer questions you may have. Take this opportunity to ask about anything that will help you better understand the recommended treatment and give you peace of mind about overcoming your POP.
Questions to ask your doctor
- How much experience do you have with treating pelvic organ prolapse?
- What are the most common side effects of the recommended treatment?
- What are the risks of the recommended treatment?
- What are the risks of no treatment? Will it get worse?
- How do I prevent my symptoms from getting worse?
Be sure to bring a list of medications, past surgeries, and medical conditions with you to the appointment. Having this information on hand may help make the visit more productive.
What to bring to the appointment
- Gynecology records
- Primary care records
- Surgery history
- Medication history
- Current medication
Symptom explanations to discuss
- When your symptoms started
- When your symptoms get worse
- Where you feel pain
- Activities or movements that make your symptoms get worse (coughing, laughing, jumping, etc.)
Treatment options to discuss
- Lifestyle changes (like diet, daily exercise)
- Pelvic floor muscle exercises (like Kegels)
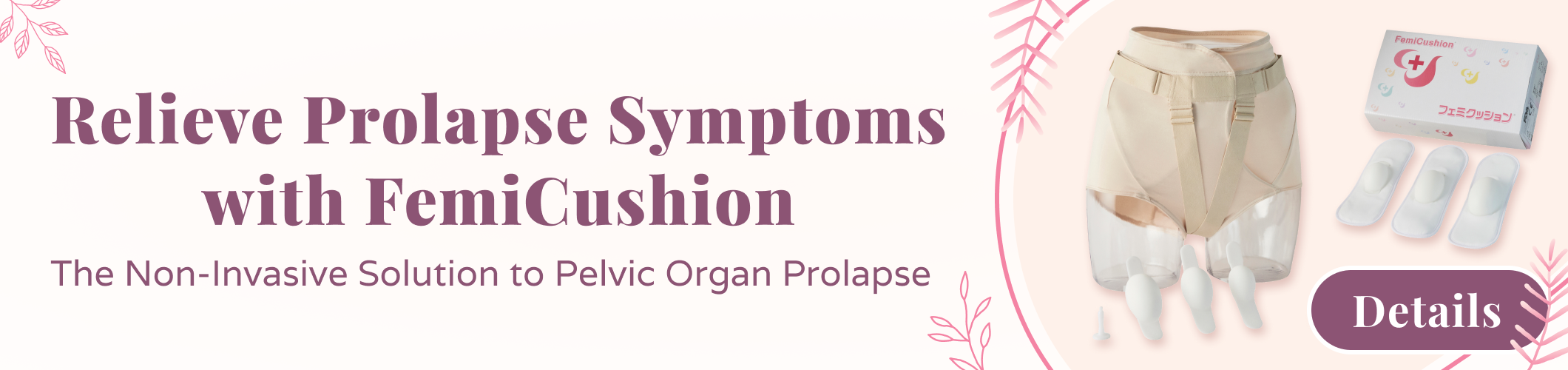
- Support pants and undergarments (like FemiCushion)
- Upside and the downside of a pessary
- Prolapse surgery pros and cons
Asking Your Doctor about FemiCushion
FemiCushion is a new treatment option for pelvic support that your doctor may not yet know about. It combines the benefits of a pessary and the simplicity of knickers. Unlike pessaries, FemiCushion is non-invasive; and unlike other over-the-counter prolapse support garments, its unique design keeps your prolapsed organs securely in your body with a patented silicone cushion.
Independent tests show that FemiCushion is an effective alternative to pessaries:
"FemiCushion presents lower risk of complications when compared to pessaries, due to the fact that it is not placed inside the vagina and it is removed daily for hygiene, reducing the risk of infections and negligence."[3] -Pelviperineology Journal, June 2016
Also, it has been found to be useful for helping with post-surgery recovery:
“The patient was discharged on the fifth day after surgery and used an external pessary (FemiCushion) for 2 months postoperatively, until the graft was firmly engrafted. This external pessary supports the pelvic floor muscle and can be used before surgery after removing a vaginal pessary, thereby improving patient quality of life. Patients can also use the external pessary if they develop sexual dysfunction while using a vaginal pessary.”[4] -The Sexual Medicine Society of North America 18th Annual Fall Scientific Meeting, October 2017
FemiCushion is effective, non-invasive, and comfortable. It provides the right amount of external support and is discreet under regular clothes because it’s worn just like underwear.
Learn more about the benefits of FemiCushion UK and its patented design by visiting the Why FemiCushion page. Learn More About FemiCushion UK
References
- https://www.nih.gov/news-events/news-releases/roughly-one-quarter-us-women-affected-pelvic-floor-disorders
- https://www.aafp.org/afp/2010/0501/p1111.html
- https://www.researchgate.net/publication/305469310_Femicushion_a_new_pessary_generation_-pilot_study_for_safety_and_efficacy
- http://smsna.org/V1/index.php?option=com_content&view=article&id=419&abstract_id=206
Disclaimer: The information on this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained on or available through this website is for general information purposes only.